Table of Content
We support all home based services, includingHome Care, Private Duty Nursing, Private Duty Non-Medical, Home and Community Based Services , Home Health, Pediatric Home Care, and Outpatient Therapy at Home. Financial metrics will provide information on revenue, days sales outstanding , gross margin, late claims, etc. Analyzing this information over a period will help home care agencies measure the agency's financial health and identify areas for improvement.
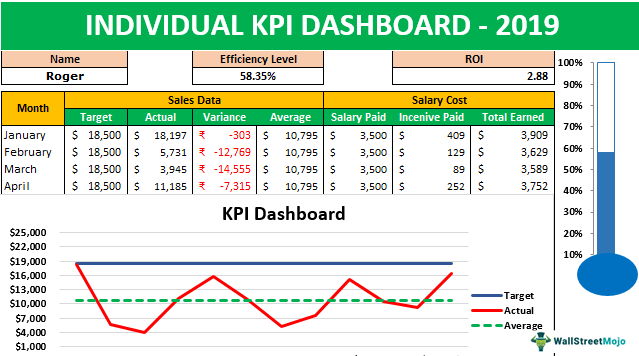
Operations Leaders at Home Care Agencies must establish processes to obtain, publish, and review these KPIs with their team members as per a cadence. This KPI can stratify revenue across different bases and identify the top revenue-producing services. The KPI should be available on the home care software by payer, location, and lines of services.
Spend less time on paperwork, billing and more time on home infusion patient care
Non-profit long-term care facilities are able to reach a higher quality of care through a more effective balance of business aspects and prioritizing resident well-being and care quality over profit maximization. Higher nurse staffing levels and fewer healthcare deficiencies are non-profits’ main strengths over for-profit organizations. The dignity with which residents are treated and the friendliness and caring of staff, especially aides, are critical prerequisites to a quality life experience. Agencies that participate in the Consumer Assessment of Healthcare Providers and Systems program can gain valuable insight into the client satisfaction and identify their improvement when this KPI is tracked over time. As home health quality measures reports are public, they can compare the results with other providers.
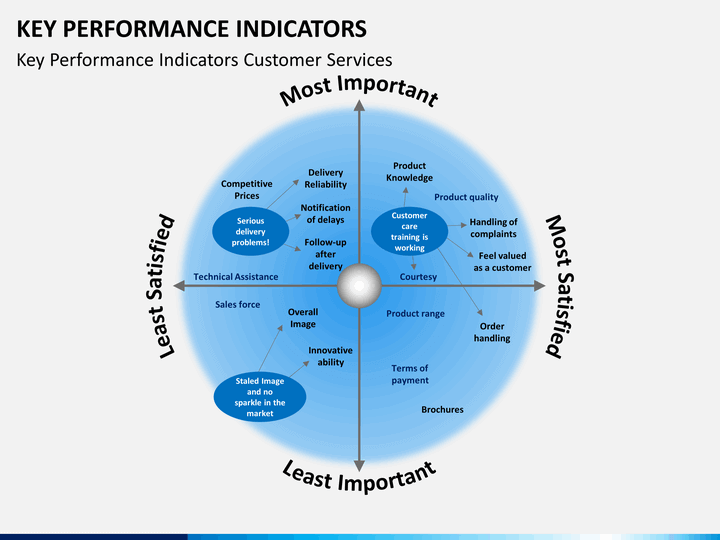
Organizations as a whole are dependent on their administration and workers of all levels and have such KPIs as client satisfaction and overall statistics of quality. Therefore, their KPIs also range from simple punctuality and lack of errors to teamwork effectiveness and rate of innovative solutions’ implementation. Measurement is the first step in identifying the opportunities for improvement.
Lecturer/Senior Lecturer in Nursing, Full time/Part Time
The only way agencies can confirm that their business objectives are being fulfilled is by tracking and measuring their performance. Home care professionals have a responsibility to deliver high-quality care every day, and so you need KPIs that measure outcomes. KPIs are also important for measuring workforce performance and business growth. Taking on more care packages often means you need your care team to increase productivity or it might be necessary to recruit more care professionals into your team to increase capacity. For instance, if a person feels that their quality of life has improved because they are getting more autonomy and independence in their lives, then that would be considered an important KPI to track.
Understanding the difference and how it fluctuates week to week can help the owner assess if they are pricing their services appropriately. In these data, the Cronbach's alpha for these seven ADL performance variables was.91, indicating a high level of internal consistency. The dependent variable was simply the difference between the ADL scale at admission and at the time of the quarterly admission. Positive values reflect decline, whereas negative values reflect improvement. The organisation is looking to set up teaching homes to provide training after participating in practice-based research to improve end of life, dementia and sensory impairment care. This metric should be available by payer, location, and lines of services.
PDPM Requires MDS Coordinators to Handle More Data
In 30 minutes we will show you how MyHelpa provides the capability you need to run a productive, efficient & compliant home care operation. You will need the tools to be able to capture the right data and analyse it accordingly. The purpose of KPIs is to make results more understandable by presenting a clear picture of what is happening in your service or organisation. To be effective, KPIs must unite the entire workforce, whether they are based mainly in the office or they are out in the field providing care. Vice-president Terri Soukup says that the AlayaCare dashboard has helped them significantly refine KPI reporting, allowing the agency to more proactively predict trends. KPIs are measurable values that reveal whether a company is achieving its objectives or not.
Other KPIs may include consistency in high-quality care, number of injuries inflicted on patients, rates of medical errors, and others. Diet, nutrition, and food service are especially important to quality of care and life for residents of a nursing home. Therapeutic diets, for instance, are vital to the physical health status of some residents . Adequate nutrition is essential to the physical health status of all residents.
In an age where data analytics and statistics drive financial decisions, how well you organize and understand your data becomes the difference between profitability and bankruptcy for long-term care facilities. This refers to the ability to convert a prospective client into a paying client. It’s overlooked for many reasons, but whatever the excuse, it needs to be monitored. For example, you should be able to identify who the best person is to answer the phone when someone calls to inquire about your services. Do they know how to communicate in a way that would convince someone to engage your agency for services? There are so many ways to do this wrong and it is so satisfying and profitable if you do it right.
KPIs need to address all aspects of a business, from the quality of care and client conversion to HR, marketing, and finance. The data collected by tracking KPIs provides statistics and enables a home healthcare agency to analyze its progress over a specific time, compare it to its industry peers and look for ways to improve its performance. By these criteria, our analyses indicate that changes in global ADL function may be of questionable utility as a performance indicator for nursing homes. Facility identity alone explained, depending on the group, only 8% to 14% of the variation in ADL functional change. Even when we added resident characteristics to facility identity, the total explained variation never exceeded 20%. The factors included in our models did not capture a minimum of 80% of the variation in functional change.
Rehabilitations and therapies follow data-driven norms to determine their expected progression. Take that data-driven calculation, and drive your admissions based on them. One of the most common reasons non-profit Skilled Nursing Facilities go out of business is the inability to predict and plan for residents’ costs. When the coverage doesn’t meet the totality of the long-term care costs, it becomes the non-profit facility’s responsibility, which can be a huge hit when resources are scarce.

Eighty-two percent of admissions were non-Hispanic White, with the next largest group of admissions being non-Hispanic Black. The majority of admissions came to the nursing homes from some type of communal living arrangement, with only 26% having lived alone prior to admission. More than half of all admissions (58%) came to the nursing home directly from an acute-care hospital. Close to a majority of admissions had had no episode of long-term care in the past 5 years, but almost 42% had had a previous stay in some nursing home during the 5 years prior to admission to this nursing home. Initial steps in the analyses included a review of the distribution and descriptive statistics for each variable. The dependent variable in these models was change in ADLs in the quarter following admission.
KPIs can also help employees focus their resources on improvements that have a direct impact on business performance, such as workforce productivity, client conversion and net change in your care team headcount. This effort differs from previous research in that we estimated models that treated each facility as a separate variable. Earlier approaches to this issue focused on specific home characteristics and assumed that those characteristics constituted the facility-level factors that affected resident outcomes. If any unmeasured home characteristics affected outcomes, then the variance attributable to those unmeasured facility characteristics was error in the model. Relatives were less stressed about the process and felt quality provided had improved. They also felt the staff had a better understanding of the pain residents were experiencing.
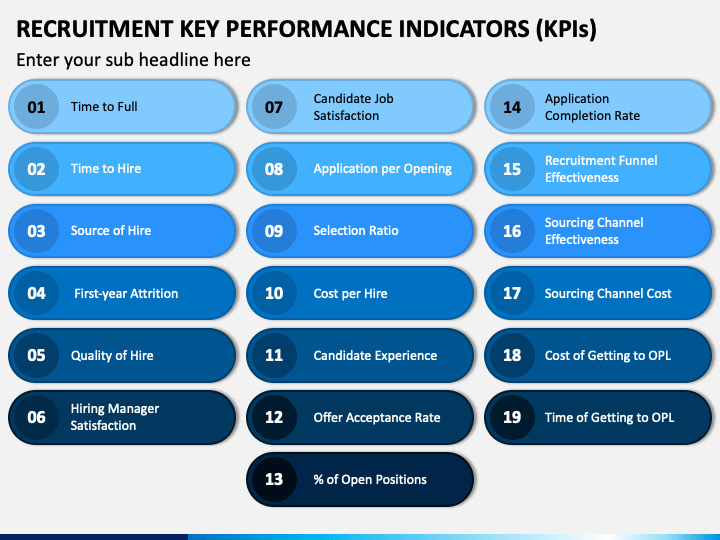
Workforce metrics such as churn rate, job applications received, 1st interviews completed, DBS checks submitted, training attended and completed, can be helpful KPIs in forward planning for growth. Similarly capturing the reasons for leaving in exit interviews can provide invaluable insight into how to improve retention. Used carefully, KPIs can also empower employees to choose which activities NOT to do, which is essential when prioritisation of an employees’ use of their time can have significant consequences on overall performance. Key Performance Indicators can help people working in home care to focus their time and efforts in the most effective ways. The AlayaCare platform was built to be continuously improved and flexible enough to shift along with an evolving industry. It offers agencies seamless access to data, advanced analytics, and reporting abilities in any area of business.
When working in the home health care industry, the well-known motto “the client should always come first” is far more than just a phrase. Monitoring the quality of care you provide is critical for your business’s success, as it can help you guarantee positive client outcomes and ensure efficient reimbursement for service. CareVoyant is a leading provider of cloud-based integrated enterprise-scale home health care software that can support all home-based services under ONE Software, ONE Patient, and ONE Employee, making it a Single System of Record. We support all home care lines of service, includingHome Care,Private Duty Nursing,Private Duty Non-Medical,Home and Community Based Services ,Home Health,Pediatric Home Care, andOutpatient Therapy. Because our cohort contained all admissions, some proportion of those admissions were readmissions to the same nursing home after an acute-care stay. Twelve percent of admissions came to the home from an acute-care setting and had had a previous stay in the admitting nursing home in the 5 years previous to this admission.

This waiver is set to expire at the end of the federal COVID-19 public health emergency, which is currently set for July. CMS has promised providers a 60-day notice prior to the end of the emergency. Hopefully, this research will stimulate discussion of this issue and the development of some reasonable standard concerning this issue. However, after the field reaches some agreement on how much a home's performance must affect an indicator for that indicator to be useful, investigators must move on and attempt to understand which indicators meet that standard.


No comments:
Post a Comment